B. Pollio, G. Delios, M. Tucciarone, M. Girotto, P. Schinco
Abstract
Central nervous bleeding emergencies are the most serious complications of Oral Anticoagulant Therapy (OAT), with an incidence of 1% per patient-year. From January 2004 through January 2010, we observed 79 episodes of anticoagulation-related acute intracranial hemorrhages (AIH) in a cohort of 76 consecutive patients reporting to our emergency department.
All patients were treated with a systematic approach: single bolus of 25-30 IU per Kilogram of Prothrombin Complex Concentrate (PCC) and intravenous administration of 10 mg of vitamin K1 within one hour after baseline CT scan of the head. All the patients simultaneously received urgent neurosurgical evaluation. Patients’ history, clinical and serological data and ongoing therapy were recorded and analysed. Functional outcomes at 90 days were assessed with the modified Rankin Scale. Median age of our cohort was 77,6 years (range 38-90) with a male-female ratio of 1,32; indications for OAT were: atrial fibrillation in 65 (82%), heart valve prostheses in 10 (13%), other indications in 4 cases (5%). 18 patients (29%) needed emergency neurosurgical intervention; 35 (44%) patients reported a recent trauma. Acute reversal of OAT (INR<1,5) was obtained in 90% of cases within 30 minutes after therapy administration. 8 subjects had non-fatal thrombotic events, (7 pulmonary embolisms and 1 ischemic stroke). Mortality rate at 90 days was 40%. Although hypertension is a well-known risk factor for intracranial hemorrhage, surprisingly in our cohort a previous history of hypertension was associated with a favourable outcome (p<0,002), possibly due to better control of blood pressure during acute bleeding. Of 48 patients alive after three months, 35 (73%) showed a Rankin score ≥4 at diagnosis, 24 (50%) at discharge and only 13 (27%) at three months. These data reveal the possibility of a remarkable margin of recovery improvement and make rapid treatment mandatory.
(»Download here full PDF version)
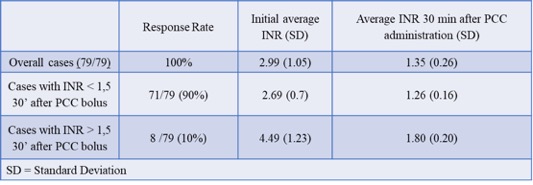
Relevance of initial INR to achieve INR <1.5

